The use of GLP-1 medications to control blood glucose levels and even weight is currently one of the most hotly debated topics in the diabetes community. These GLP-1 agonists, more commonly referred to as Ozempic, Mounjaro, or Semaglutide, have made headlines due to their use by celebrities and rapid weight loss in non-diabetics. But how does it function? Is it really beneficial to people with diabetes of any kind? And should you think about it? This blog post will break down the basics of GLP-1 agonists, real experiences, and more.
What is GLP-1?
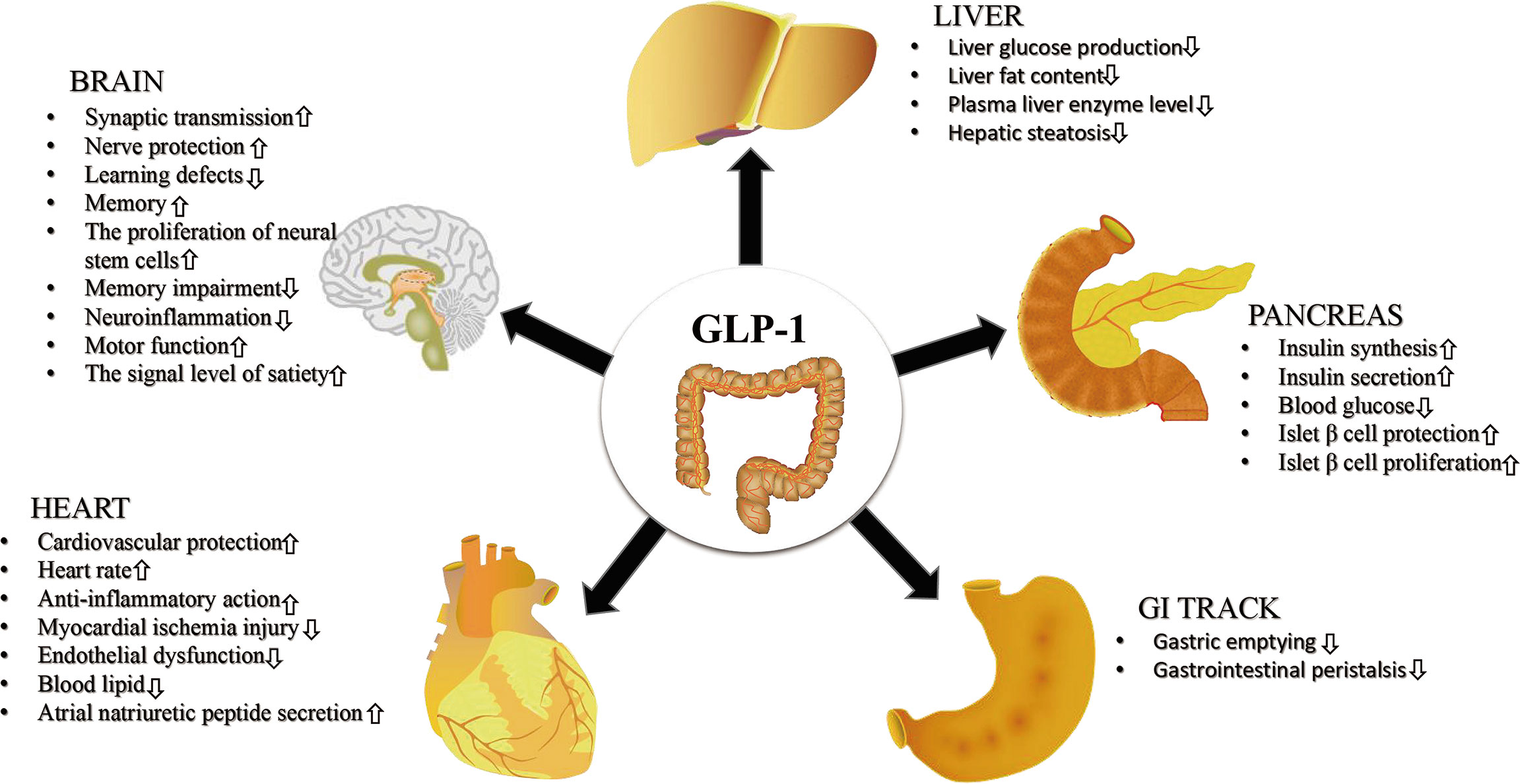
GLP-1, short for glucagon-like peptide-1, is a natural hormone your body makes in the gut after you eat. It is pretty clever at what it does: it tells your pancreas to release insulin when your blood sugar goes up, slows down the rate at which food leaves your stomach, and even tells your brain to feel full sooner. Together, these actions help keep blood sugar steady and reduce overeating.
Scientists have created medicines that copy the effects of this hormone, known as GLP-1 receptor agonists. Semaglutide, a medication that mimics GLP-1 but lasts much longer in the body than the hormone itself, is one of the most effective. Ozempic is the brand name for semaglutide, which is prescribed to people with type 2 diabetes. If you’ve heard of it, it’s just the brand name. Ozempic lowers blood sugar, lowers the risk of certain heart conditions, and frequently provides weight loss as an added benefit. Snehal’s Experience
My insulin requirements, appetite, and weight have always been a balancing act as someone who has type 1 diabetes for the past 23 years. My HbA1c has typically remained within the range of 6.2 and 7, which is regarded as excellent control. During my annual routine tests this year (find out more about routine tests here), I noticed that my cholesterol had increased and that I was beginning to show signs of frozen shoulder. I was also 89 kg—overweight for me. My doctor suggested Rybelsus (oral semaglutide) to help with weight management, which in turn would help reduce cholesterol. I started taking a 3 mg dose in April 2025.
Within two weeks, my appetite had dropped almost by half. My daily insulin doses were reduced as well, but adjusting at first was a nightmare. I wasn’t sure how much I should eat or inject in terms of insulin. I tried my “sick day” logic (read the sick day management protocol here)—reduce by 2-4 units and ended up with severe hypos all day (read our hypo guide here). To put it mildly, it was depleting. After a lot of trial and error, I figured out what worked for me. My daily insulin requirement eventually reduced by about 35–40 %.
In just two weeks, the weight went from 89 kilograms to 84 kilograms. However, it wasn’t an easy ride. I started to feel uneasy in my stomach, yawning whenever I thought of food, having to burp, and feeling constantly nauseous throughout the day. After meals, a few Diet Pepsi sips seemed to calm it down. I also tried some home remedies to soothe my tummy, which didn’t help much.
I also started peeing a little bile—also known as “pitt” in Marathi—in the mornings while brushing my teeth by the fourth week. Some days I skipped my dose because my stomach felt off.
Then came a frightening incident. Things spiraled when I had an early morning flight, which meant less sleep and less stress about the trip. During the flight, I continued to vomit bile while at the airport. That day, I didn’t go to Rybelsus, and it showed. Throughout my trip, I was uneasy and couldn’t eat anything. At that point, I ate lemon juice, a lot of cucumber, and simple rice dishes like dal chawal or khichdi, which felt like comfort food to me. I updated my doctor about my situation, and they advised me to stop Rybelsus for a while; avoid tea, coffee, fizzy drinks, alcohol, and take antacid medication twice a day.
Additionally, we decided that I should stop Rybelsus a day before traveling. After this experience, I took a break for almost a month. Keep in mind that Rybelsus has a long-lasting effect even after you stop taking it. When I had to travel early again, the pattern repeated even though I’d stopped Rybelsus the day before. I have since completely stopped taking Rybelsus and am waiting to talk with my doctor about the next steps. In 4-5 months, with breaks in between, I lost about 10 kg. Due to Rybelsus, I have continued to exercise three to four times per week and consumed very little food. Here’s what I’ve figured out so far :
The entire time, I was taking the 3 mg dose. I wrote about my experience in a journal, noting when I had problems and how my body felt. This helped me have better discussions with my doctor.
Rybelsus definitely suppressed my appetite and helped me lose weight.
It also slowed my stomach emptying; after restarting after a break, I began noticing late post-meal glucose spikes on my CGM, 3-4 hours after eating. You can view the video playlist and read our blogs about diabetes technology in India here. Rybelsus, traveling, not getting enough sleep, stress, and traveling are not good for me. They made the nausea/bile episodes worse. To lessen the likelihood of an episode, I now stop Rybelsus one day before traveling. Read our blogs on travel & diabetes here and see the video playlist here.
I haven’t had much alcohol, but when I was taking Rybelsus, I didn’t feel like drinking much—now I just have a glass of wine every now and then. Despite my love of Americanos, I also didn’t feel like drinking coffee, which was surprising. The pill is to be taken on an empty stomach first thing in the morning. Recommended wait time before eating anything is 30 mins, but I feel uneasy at 20 mins, so I eat something light like a cucumber or a moong-besan chilla after 15-20 mins. (As talked about with my doctor) PS: Did you know that the Blue Circle Diabetes app or this link can be used to look up the macros of any food? Due to the drastic reduction in your food intake, you may also experience constipation. Keeping hydrated is helpful. I continue to drink more than four liters of water each day. Make sure you get enough protein, iron, and micronutrients because rapid weight loss can cause problems like hair loss and deficiencies in nutrients. Everyone’s experience with GLP-1 drugs is different. I’ve talked to a lot of people who manage the mild nausea with easy home remedies. For me, the side effects were intense enough to need breaks and medical advice.
If you have a history of bloating, burping, or acid reflux, or live with type 1 diabetes like me, keep a close eye on your blood sugars and stomach symptoms.
Keep a symptom diary, work with your doctor, start slowly, and don’t ignore severe nausea or bile vomiting. Sometimes breaks help your gut recover; sometimes a different approach or dose is needed.
I’m still figuring out what balance works for me. Rybelsus has been a powerful tool, but not an easy one. My hope in sharing this is to give a real-life glimpse of both the benefits and the bumps along the way.
Please keep in mind that Rybelsus, like other GLP-1 medications, may cause additional side effects, such as the worsening of diabetic retinopathy. Always read the patient information leaflet that comes with your medication and discuss any concerns with your doctor.
Nishtha’s Experience
As part of my condition, I deal with severe insulin resistance and live with type 1.5 diabetes. I quickly gained weight after starting insulin therapy and continuing on Metformin, gaining over 30 kilograms in about four years. It became a vicious cycle—I’d put on weight, would have to increase my insulin dosage, which would make losing weight harder. Despite my 5’8″ frame, nearly 90 kgs was a problem figure.
- My weighing machine would not move at all regardless of how much I exercised at home, in the gym, or by swimming. I could live with the extra weight, but it also increased my need for insulin and increased my risk of heart disease. To me, that was unacceptable. I read more about “Ozempic” as I looked into ways to get around this problem. At this point, it was already being touted as the weight loss drug Hollywood swears by, but on reading further, I realised it was meant to be used in treatments for type 2 diabetes. More importantly, I decided to inquire about it after reading about how it affected my ability to control HbA1c levels. While it’s not typically used for insulin-dependent diabetics, doctors can prescribe it to you in case of insulin resistance.
- While Ozempic wasn’t officially available in India just yet, my doctor informed me Rybelsus, a semaglutide, had been available for close to a decade here. I started using it with her blessing. You should take 3 mg for the first month, which is also known as the “wash-in period.” Your body will be able to better acclimate to the medication at a lower dose, and the side effects will be relatively milder. I did deal with acidity, constipation, and severe loss of appetite around the first month. But it was to be expected. I increased my dosage to 7 mg the following month, particularly after training myself to eat better and occasionally taking it. After a few months of this, my weight started to drop and my blood glucose stability began to significantly improve.










